肾的先天性畸形,肾脏可以发生多种多样的畸形,畸形的肾脏对其他器官可以产生压迫,肾脏本身则可以发生感染、出血、结石,也可导致肾实质性或肾血管性高血压,严重的肾实质减少,则发生肾衰竭。肾不发育可发生在一侧或两侧。额外肾是单独存在的第三个肾脏,为泌尿系最罕见的畸形,发生在左侧为多。
肾结构异常:(一)肾发育不全指肾脏小于正常体积的50%以上,但肾单位及导管的分化和发育是正常的,只是肾单位的数目减少,故肾小盏及肾小叶的数目也减少。1、单纯性肾发育不全:属非遗传性畸形,多数是散发的,个别有家族性,无性别差异。2、节断性肾发育不全:多见于女性,无家族性。从肾被膜外可见肾实质菲薄的部位,该处的肾小管萎缩,充满胶样管型,仅有极少数肾小球,可见残留的髓质。3、少而大的肾单位肾发育不全:多见于男性,常是双侧性,无家族性。
(二)囊性肾发育异常:即多房性肾囊性变,常为单侧性,无家族性,无性别差异。其病因是胎儿早期输尿管梗阻的最严重后果。
(三)多囊肾系遗传性疾病,两侧肾脏弥漫性病变,体积增大,满布大小不等的囊肿,无明显的肾实质发育不全,但由于囊肿压迫肾组织亦可使肾功能受损。1.婴儿型多囊肾属常染色体隐性遗传,其病因不明。发病不限于婴儿,亦可发生在儿童和成人。伴随的肝脏病变为先天性肝纤维化。2.成人型多囊肾属常染色体显性遗传,是肾脏囊性疾病中最常见的一种。双肾弥漫性进行性囊性病变,高血压,出现血尿,肾钙质沉着,进行性肾功能衰竭,急性腰痛。除非进行透析或肾移植,一般在60多岁时死亡。
(四)单纯性肾囊肿:孤立性或多发性,常见于50岁以上成年男性及左肾,故可能是后天性的,囊肿常是孤立的,单侧病变,但可合并对侧肾病变。囊肿自肾实质产生,而不与肾盏或肾盂相通,其大小不一,直径由2~3cm至10cm不等。周围的肾实质被压迫而呈一薄壁,囊壁与肾实质紧密贴合不易剥离。囊内为浆液,含少量的乳酸脱氢酶、氯化物、蛋白与脂肪、胆固醇结晶及少量尿液,如有出血则含血性液。临床常无症状,可因腹部肿物在超声检查或排泄性尿路造影时被偶然发现,显示肾盂肾盏受压、拉长及变形。一般不需治疗,继续观察。如有严重压迫症状,可行囊肿去顶术或肾部分切除术。如有感染、结石、肿瘤与肾盂相通等并发症,或肾有高度损害,则考虑肾切除术。
(五)髓质海绵肾:又称髓质集合管扩张症或称Cacchi-Ricci病。系指一侧或双侧肾内单个或多个锥体内集合管的囊性扩张。认为是先天性异常,其发病机理尚未阐明。有三种病因假设,可能与感染、梗阻、遗传有关。
(六)肾多房性囊肿其病理特点是大而具有完整被膜的肿物,将正常肾组织推移并压迫萎缩。切面可见由很多囊肿构成,囊肿直径达数毫米至数厘米,内含草黄色或血性液体。囊壁被覆规则的扁平及立方上皮细胞。
(七)髓质囊性病:包括常染色体显性遗传的髓质囊性病和常染色体隐性遗传的familialjuvenilenephrophthisis。其特征是肾髓质有多发囊肿,呈慢性进行性肾功能不全,至青少年期出现尿毒症;但也有呈良好状态达成年的病例。肾脏较正常为小,髓质有许多囊肿,其直径自1毫米至1厘米,囊肿被覆扁平上皮。其余肾组织可见肾小球数目减少,肾小管萎缩及肾间质细胞弥漫性纤维化,慢性炎细胞浸润。均在儿童期出现症状,表现为多尿、烦渴及发育迟滞。
肾位置、形态、旋转及血管异常:(一)异位肾胎儿期肾胚芽位于盆腔内,随着发育肾逐渐上升到正常位置,若上升发生障碍或过度上升,或误升向对侧,即形成异位肾。可位于盆腔、髂部、腹部、胸部和对侧或交叉。1.盆腔肾:其发生率为500~1200人中有1例。肾较小,呈扁平、球形、并有一定程度的向前旋转;输尿管也较短,有轻度曲折,肾功能正常,但易于并发尿路梗阻、结石、感染而引起症状,主要为疼痛、血尿、排尿困难、膀胱刺激症、腹部肿块和胃肠症状。无症状的异位肾不需任何治疗,如有并发症则进行相应的处理。2.胸内肾:很少见,左侧及男性略多,可发现于任何年龄。除有肾血管异常外,还并发有先天性膈疝,缺损小者只能通过肾蒂而无其他脏器进入胸腔内。一般无症状,在体检或胸部X线检查时发现膈上有肿物。肾盂造影可以确诊,毋需治疗。3.交叉异位肾:一侧肾脏由原侧跨越中线移位至对侧,而其输尿管仍位于原侧。可分为融合型和非融合型,前者较多见,异位肾一般低于正常侧,肾盂位于肾的前面,输尿管仍从原有径路进入膀胱,开口于正常部位。常合并其他泌尿系畸形。多数无症状,或有下腹痛、肿块及压迫症状。
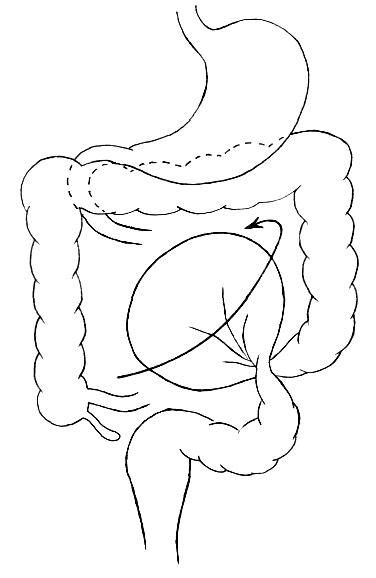
(二)融合肾:由于原始肾组织块的分裂停顿或发育异常、两侧肾脏相互融合,完全性或部分性,有各种类型如蹄铁形肾、乙状肾、盘形肾、块肾等。由于融合发生于胚胎早期,因而均伴有所处的位置异常和肾旋转不良。其血供可来自骶中动脉和髂总动脉。蹄铁形肾在融合肾中最常见,大约每400人中有1例,多见于男性。
(三)肾旋转异常:在正常发育过程中,肾轴应发生90°旋转。可发生4种旋转异常:腹侧旋转(未旋转),腹中向旋转(旋转不全),侧向旋转(反向旋转)和背侧旋转(旋转过度)。最多见的是旋转不全,即肾盂朝向前方;如旋转过度,则肾盂朝向后侧。尿路造影可明确诊断,如无并发症存在毋需治疗。
(四)肾血管异常:原始的肾脏血管来自骶中动脉,髂动脉或低位腹主动脉。在正常发育下,原有的血管逐渐萎缩而代以肾动脉。如原始供应血管持续存在,则可成为肾血管异常原因之一。或成为肾或输尿管的副血管。多见于输尿管的前方或肾盂输尿管连接处附近。常可影响或阻碍尿液排泄。而供应肾上极的异常血管则不致造成尿路梗阻。在临床上,肾血管异常除可产生输尿管梗阻外,无其他重要意义。