2008年7月31日星期四
五官 Glomus tympanicum 鼓室球瘤
Glomus bodies in the middle ear are situated along Jacobson's nerve (a branch of CN IX,鼓室神经) which forms the tympanic plexus. Branches of the tympanic plexus (and potential locations for glomus tympanicum tumors) occur on the cochlear promontory, near the round window, eustachian tube egress, tensor tympani tendon and along the inferior tympanic canaliculus. The classic location is the cochlear promontory.
On CT, the tumors are typically small, do not erode the bone (as opposed to cholesteatomas). On MR they demonstrate marked enhancement. Larger tumors may have a 'salt and pepper' appearance caused by flow voids in the mass.
Glomus tumors occur (in order of frequency) at the jugular foramen, branches of the vagus nerve (Arnold's nerve), carotid bulb or hypotympanum.
Overall glomus tumors are multiple in 15% of patients.
http://education.auntminnie.com/QMachine.ASP?UID=25I0TGNP&PageId=5&Sess=4437525
2008年7月28日星期一
骨骼 多发性基底细胞痣综合征
多发性基底细胞痣综合征 为家族性,属于常染色体显性遗传病。其特征是:多发性基底细胞痣或基底细胞癌、颌骨多发性囊肿、肋骨畸形、颅内钙化。临床表现为:①颌骨牙源性角化囊肿(下颌骨多于上颌骨,单发或多发,常为双颌同时累及);②痣样基底细胞癌(主要发生于面部、颈部、躯干上部、眶周、眼睑、鼻、颧突等部位;上唇为面部最常发部位,一般为单侧。多数病损处于静止状态);③肋骨畸形(包括分叉肋、融合肋、肋骨发育不全或部分缺失);④颅内钙化(最常见为大脑镰钙化,其次为小脑幕钙化)。
与常染色体显性遗传有关,外显率高达95%。本综合征特点有:多发性痣样基底细胞上皮瘤、多发性颌骨囊肿、分杈肋及其他骨骼异常、中枢神经系统改变。本病患者可出现颅内钙化,头颅CT扫描可见大脑镰、小脑幕、硬脑膜及基底节区出现钙化灶。
Radiologic Overview of the Diagnosis:
Basal cell nevus syndrome:
Key radiographic findings in basal cell nevus syndrome include odontogenic keratocysts (as described above), rib anomalies, vertebral anomalies, dural calcifications, and short metacarpals. These patients are at increased risk for medulloblastoma and cardiac and ovarian fibromas.
Key Points:
Multiple odontogenic keratocysts should raise concern for the possibility of basal cell nevus syndrome (Gorlin-Goltz syndrome).
This syndrome is a genetic condition characterized by multiple nevoid basal cell carcinomas.
Basal cell nevus syndrome has several other associations including: odontogenic keratocysts, dural calcifications, rib and vertebral anomalies, short metacarpals, and midface hypoplasia.
These patients are at increased risk for medulloblastoma and cardiac and ovarian fibromas.
http://education.auntminnie.com/QMachine.ASP?UID=25G14GM7&PageId=5&Sess=6977960
2008年7月26日星期六
泌尿 肾的先天性畸形
肾结构异常:(一)肾发育不全指肾脏小于正常体积的50%以上,但肾单位及导管的分化和发育是正常的,只是肾单位的数目减少,故肾小盏及肾小叶的数目也减少。1、单纯性肾发育不全:属非遗传性畸形,多数是散发的,个别有家族性,无性别差异。2、节断性肾发育不全:多见于女性,无家族性。从肾被膜外可见肾实质菲薄的部位,该处的肾小管萎缩,充满胶样管型,仅有极少数肾小球,可见残留的髓质。3、少而大的肾单位肾发育不全:多见于男性,常是双侧性,无家族性。
(二)囊性肾发育异常:即多房性肾囊性变,常为单侧性,无家族性,无性别差异。其病因是胎儿早期输尿管梗阻的最严重后果。
(三)多囊肾系遗传性疾病,两侧肾脏弥漫性病变,体积增大,满布大小不等的囊肿,无明显的肾实质发育不全,但由于囊肿压迫肾组织亦可使肾功能受损。1.婴儿型多囊肾属常染色体隐性遗传,其病因不明。发病不限于婴儿,亦可发生在儿童和成人。伴随的肝脏病变为先天性肝纤维化。2.成人型多囊肾属常染色体显性遗传,是肾脏囊性疾病中最常见的一种。双肾弥漫性进行性囊性病变,高血压,出现血尿,肾钙质沉着,进行性肾功能衰竭,急性腰痛。除非进行透析或肾移植,一般在60多岁时死亡。
(四)单纯性肾囊肿:孤立性或多发性,常见于50岁以上成年男性及左肾,故可能是后天性的,囊肿常是孤立的,单侧病变,但可合并对侧肾病变。囊肿自肾实质产生,而不与肾盏或肾盂相通,其大小不一,直径由2~3cm至10cm不等。周围的肾实质被压迫而呈一薄壁,囊壁与肾实质紧密贴合不易剥离。囊内为浆液,含少量的乳酸脱氢酶、氯化物、蛋白与脂肪、胆固醇结晶及少量尿液,如有出血则含血性液。临床常无症状,可因腹部肿物在超声检查或排泄性尿路造影时被偶然发现,显示肾盂肾盏受压、拉长及变形。一般不需治疗,继续观察。如有严重压迫症状,可行囊肿去顶术或肾部分切除术。如有感染、结石、肿瘤与肾盂相通等并发症,或肾有高度损害,则考虑肾切除术。
(五)髓质海绵肾:又称髓质集合管扩张症或称Cacchi-Ricci病。系指一侧或双侧肾内单个或多个锥体内集合管的囊性扩张。认为是先天性异常,其发病机理尚未阐明。有三种病因假设,可能与感染、梗阻、遗传有关。
(六)肾多房性囊肿其病理特点是大而具有完整被膜的肿物,将正常肾组织推移并压迫萎缩。切面可见由很多囊肿构成,囊肿直径达数毫米至数厘米,内含草黄色或血性液体。囊壁被覆规则的扁平及立方上皮细胞。
(七)髓质囊性病:包括常染色体显性遗传的髓质囊性病和常染色体隐性遗传的familialjuvenilenephrophthisis。其特征是肾髓质有多发囊肿,呈慢性进行性肾功能不全,至青少年期出现尿毒症;但也有呈良好状态达成年的病例。肾脏较正常为小,髓质有许多囊肿,其直径自1毫米至1厘米,囊肿被覆扁平上皮。其余肾组织可见肾小球数目减少,肾小管萎缩及肾间质细胞弥漫性纤维化,慢性炎细胞浸润。均在儿童期出现症状,表现为多尿、烦渴及发育迟滞。
肾位置、形态、旋转及血管异常:(一)异位肾胎儿期肾胚芽位于盆腔内,随着发育肾逐渐上升到正常位置,若上升发生障碍或过度上升,或误升向对侧,即形成异位肾。可位于盆腔、髂部、腹部、胸部和对侧或交叉。1.盆腔肾:其发生率为500~1200人中有1例。肾较小,呈扁平、球形、并有一定程度的向前旋转;输尿管也较短,有轻度曲折,肾功能正常,但易于并发尿路梗阻、结石、感染而引起症状,主要为疼痛、血尿、排尿困难、膀胱刺激症、腹部肿块和胃肠症状。无症状的异位肾不需任何治疗,如有并发症则进行相应的处理。2.胸内肾:很少见,左侧及男性略多,可发现于任何年龄。除有肾血管异常外,还并发有先天性膈疝,缺损小者只能通过肾蒂而无其他脏器进入胸腔内。一般无症状,在体检或胸部X线检查时发现膈上有肿物。肾盂造影可以确诊,毋需治疗。3.交叉异位肾:一侧肾脏由原侧跨越中线移位至对侧,而其输尿管仍位于原侧。可分为融合型和非融合型,前者较多见,异位肾一般低于正常侧,肾盂位于肾的前面,输尿管仍从原有径路进入膀胱,开口于正常部位。常合并其他泌尿系畸形。多数无症状,或有下腹痛、肿块及压迫症状。
(二)融合肾:由于原始肾组织块的分裂停顿或发育异常、两侧肾脏相互融合,完全性或部分性,有各种类型如蹄铁形肾、乙状肾、盘形肾、块肾等。由于融合发生于胚胎早期,因而均伴有所处的位置异常和肾旋转不良。其血供可来自骶中动脉和髂总动脉。蹄铁形肾在融合肾中最常见,大约每400人中有1例,多见于男性。
(三)肾旋转异常:在正常发育过程中,肾轴应发生90°旋转。可发生4种旋转异常:腹侧旋转(未旋转),腹中向旋转(旋转不全),侧向旋转(反向旋转)和背侧旋转(旋转过度)。最多见的是旋转不全,即肾盂朝向前方;如旋转过度,则肾盂朝向后侧。尿路造影可明确诊断,如无并发症存在毋需治疗。
(四)肾血管异常:原始的肾脏血管来自骶中动脉,髂动脉或低位腹主动脉。在正常发育下,原有的血管逐渐萎缩而代以肾动脉。如原始供应血管持续存在,则可成为肾血管异常原因之一。或成为肾或输尿管的副血管。多见于输尿管的前方或肾盂输尿管连接处附近。常可影响或阻碍尿液排泄。而供应肾上极的异常血管则不致造成尿路梗阻。在临床上,肾血管异常除可产生输尿管梗阻外,无其他重要意义。
2008年7月24日星期四
泌尿 肾周淋巴管扩张 Renal lymphangiectasia
European Journal of Radiology Extra 63 (2007) 61–63 已下载
泌尿 肾脏外伤分级
Hematuria with normal imaging studies
Contusions
Nonexpanding subcapsular hematomas
Grade 2
Nonexpanding perinephric hematomas confined to the retroperitoneum
Superficial cortical lacerations less than 1 cm in depth without collecting system injury
Grade 3
Renal lacerations greater than 1 cm in depth that do not involve the collecting system
Grade 4
Renal lacerations extending through the kidney into the collecting system
Injuries involving the main renal artery or vein with contained hemorrhage
Segmental infarctions without associated lacerations
Expanding subcapsular hematomas compressing the kidney
Grade 5
Shattered or devascularized kidney
Ureteropelvic avulsions
Complete renal laceration or thrombus of the main renal artery or vein
http://radiographics.rsnajnls.org/cgi/content/full/21/3/557
Renal injuries can be classified into fourlarge categories based on imaging findings.
Category I renal injuriesinclude minor cortical contusion, subcapsular hematoma, minor lac-eration with limited perinephric hematoma, and small cortical infarct.
Category II lesions include major renal lacerations extending to themedulla with or without involvement of the collecting system and seg-mental renal infarct.
Category III lesions are catastrophic renal injuriesand include multiple renal lacerations and vascular injury involving therenal pedicle.
Category IV injuries are ureteropelvic junction injuries.
泌尿 特发性腹膜后纤维化
DDX:淋巴瘤 腹膜后淋巴瘤范围广,显示为大结节性肿块,密度不均,可伴有肠系膜淋巴结肿大,主动脉与椎体间距增大。
DDX:转移性淋巴结及转移性肿瘤 缺乏纤维组织,表现不为连续的主动脉旁肿块或淋巴结肿大。增强后肿块不均匀强化呈结节状。
另:
低密度淋巴结:结核,睾丸癌
高密度淋巴结:Kaposi肉瘤
广泛钙化淋巴结:Castleman‘s病
泌尿 腹膜后肿瘤分类及特性
2008年7月21日星期一
骨骼 Scheuermann's disease 少年性椎体骨软骨病
The etiology of Scheuermann's disease is unknown. Possible causes include underdevelopment of the anterior spine, congenital end-plate weakness, or repetitive microtrauma.
泌尿 肾积水时IVP的一些征象
梗阻性肾影:急性梗阻时,肾实质密度增加,肾盂肾盏延迟显影。(高位梗阻优甚)
新月形肾盏:肾盏明显扩张,肾脏集合管受压、重排,肾脏外新月形影,点状影。
泌尿 Fraley syndrome

 a. Intravenous urography (nephrotomogram) showing slight fullness of the right upper pole calyces, with an associated lucency crossing the left upper pole infundibulum. b. Abdominal aortogram shows an artery (arrow) in the position corresponding to the lucency seen on intravenous urography, confirming the diagnosis of Fraley'syndrome.
a. Intravenous urography (nephrotomogram) showing slight fullness of the right upper pole calyces, with an associated lucency crossing the left upper pole infundibulum. b. Abdominal aortogram shows an artery (arrow) in the position corresponding to the lucency seen on intravenous urography, confirming the diagnosis of Fraley'syndrome.2008年7月20日星期日
中枢 不典型畸胎样/横纹肌样瘤
原发性不典型畸胎样/横纹肌样瘤(Atypical Teratoid / Rhabdoid Tumor, AT/RT )属于胚胎性肿瘤的一个亚类,是非常罕见的中枢神经系统的高度恶性的肿瘤,常发生于儿童。具有高度侵袭性及在CNS播散的潜力。其成分复杂,含有多个胚层,包括横纹肌瘤样细胞、原始神经外胚层肿瘤(PNET)细胞、间充质纺锤形样肿瘤细胞和/或上皮型肿瘤细胞,因此命名为不典型畸胎样/横纹肌样瘤。
由于其组织成分与PNET有较多重叠,过去多误诊为PNET/髓母细胞瘤或其它肿瘤(脑膜瘤等),近来由于免疫组织化学技术及分子基因技术的发展,通过特定的免疫组化标记物能够将AT/RT与其它肿瘤鉴别开来,包括EMA、vimentin、actin、hSNF5/INI1染色及基因分析。 94%在脑内,幕下多见,亦可位于幕上或椎管内。肿瘤体积常较大,易坏死、囊变、出血; 肿瘤供血丰富,常可见小流空的肿瘤血管信号影; 肿瘤强化明显,多呈环形强化,近正常脑组织面强化较内侧面更明显,也可呈实质性明显强化。 常发生脑脊液播散性转移至脑室、脊髓(24%)。 预后极差,1年及5年存活率分别为71%及28%。
鉴别诊断: PNET 髓母细胞瘤 胶质母细胞瘤 脑膜瘤等
呼吸 Congenital Lobar Emphysema
 Marked hyperexpansion of left upper lobe with collapse of left lower lobe and mediastinal shift.
Marked hyperexpansion of left upper lobe with collapse of left lower lobe and mediastinal shift.Progressive overdistension of lobe at birth
Male predominance 3:1
Associated with CHD in 15% (PDA,VSD)
Symptoms: respiratory distress (90%) and cyanosis <>
LUL 43%,RML 35%,RUL 20%,Two lobes involved 5%
X-ray Appearance
2008年7月19日星期六
呼吸 仰卧位时气胸的判定 deep sulcus sign
 Supine chest radiograph of a neonate illustrates the deep sulcus sign with abnormal deepening and lucency of the left lateral costophrenic angle (*). Findings on right lateral decubitus chest radiograph (not shown) confirmed the presence of a pneumothorax on the left side.
Supine chest radiograph of a neonate illustrates the deep sulcus sign with abnormal deepening and lucency of the left lateral costophrenic angle (*). Findings on right lateral decubitus chest radiograph (not shown) confirmed the presence of a pneumothorax on the left side. Supine chest radiograph demonstrating signs of a right supine pneumothorax despite the presence of a chest drain. There is abnormal lucency over the lower right chestand upper abdomen. Subpulmonic air (white asterisk) out-lines the inferior surface of the lung with sharp delineationof the right hemidiaphragm. The right side of the medias-tinum is unusually well defined (black arrows) because of theadjacent air rather than normal aerated lung. The deepsulcus sign is also seen (white arrow).
Supine chest radiograph demonstrating signs of a right supine pneumothorax despite the presence of a chest drain. There is abnormal lucency over the lower right chestand upper abdomen. Subpulmonic air (white asterisk) out-lines the inferior surface of the lung with sharp delineationof the right hemidiaphragm. The right side of the medias-tinum is unusually well defined (black arrows) because of theadjacent air rather than normal aerated lung. The deepsulcus sign is also seen (white arrow).血管 CLASSIFICATION OF RIB NOTCHING
1. High aortic obstruction
a. Aortitis
b. Coarctation of aorta---most common
c. Coarctation of aorta involving left subclavianartery or anomalous right subclavian artery(unilateral)
2. Low aortic obstruction (eg, aortic thrombosis)
3. Subclavian artery obstruction
a. Blalock-Taussig operation (unilateral)
b. Pulseless disease (eg, Takayasu’s arteritis); ad-vanced arteriosclerosis
4. Pulmonary oligemia
a. Absent pulmonary artery (unilateral)
b. Ebstein’s anomaly
c. Emphysema
d. Pseudotruncus arteriosus
e. Pulmonary valvular stenosis or atresia
f. Tetralogy of Fallotg
VENOUS
1. Obstruction of superior vena cava, innominate orsubclavian vein
ARTERIOVENOUS
1. Arteriovenous fistula of chest wall (intercostal ar-tery—vein)
2. Pulmonary arteriovenous fistula
NEUROGENIC
1. Intercostal neurofibroma or neurilemmoma
2. Neurofibromatosis (type 1) ---Second common
3. Bulbar poliomyelitis; quadriplegia
OSSEOUS
1. Hyperparathyroidism
2. Osteodysplasty (Melnick-Needles syndrome)
3. Thalassemia
MISCELLANEOUS
1. Idiopathic; normal variant
2. Indwelling catheter
Coarctation of the aorta is the classic cause for this etiology but normally appears bilaterally and affects ribs 4-8 due to hypertrophy and tortuosity of the intercostal arteries. The first two ribs should be uninvolved because the first and second intercostal arteries are supplied by the superior intercostal branch of the costocervical trunk.
Nuerofibromatosis Type 1 is a second common etiology for rib notching with the development of intercostal neurofibromas causing the appearance. This is the number one non-vascular etiology.
呼吸 肺先天性囊性腺瘤样畸形 CCAM
Pathogenetically, congenital cystic adenomatoid malformation has been attributed to an overgrowth of bronchioles, with almost complete suppression of alveolar development between the 7th and 10th weeks of embryonic life
CCAM is a congenital anomaly of the terminal brochioles which results in a dysplastic, multicystic mass. These cysts usually communicate with the bronchial tree. At birth, these cysts are fluid-filled. Ultimately, communication with the airway allows for the fluid-filled mass to become air-filled. Whether fluid-filled or air-filled, the cysts become increasing larger, exert mass effect, compress mediastinal structures and lung parenchyma.
CCAM consists of a multicystic intralobar mass of disorganized lung tissue, derived primarily from bronchioles. It can involve an entire lobe. Lower lobes are most often involved, but any lobe can be affected. The treatment of choice is excision of the affected lobe.
Infants less than one year old usually present with respiratory distress. Usually, the abnormality is confined to one lobe. There are three types of CCAM:
Type I: Single/multiple cysts > 2cm (most common).
Type II: Smaller cysts <2cm with mixed solid component.
Type III: Solitary solid mass.
Radiological differential diagnosis: Congenital diaphragmatic hernia, congenital lobar emphysema, localized persistent pulmonary interstitial emphysema and pneumatocele.
Treatment: Surgical lobectomy is curative with Type I. There is increased morbidity and mortality with Type II and II because the lesions are often larger at presentation.
http://www.radpod.org/2008/02/28/congenital-cystic-adenomatoid-malformation/
http://www.uhrad.com/pedsarc/peds069.htm
http://radiographics.rsnajnls.org/cgi/content/full/24/1/e17
呼吸 Kartagener syndrome 支扩、副鼻窦炎、右位心三联征
Recurrent respiratory tract infections secondary to abnormal respiratory mucociliary function because of a generalized deficiency of dynein arms of cilia. Will also affect auditory epithelium and sperm tails. Diagnosed by triad of Situs inversus (including dextrocardia), sinusitis, and bronchiectasis(1.)
Kartagener's syndromeAlso known as:Afzelius’ syndrome,Kartagener’s triad,Zivert's syndrome,Zivert-Kartagener triad
Synonyms:Immotile cilia syndrome, ciliary dyskinesia, bronchiectasis-dextrocardia-sinusitis, sinusitis-bronchiectasis-situs inversus syndrome, situs inversus-sinusitis-bronchiectasis, dextrocardia-bronchiectasis-sinusitis immotile cilia, dextrokardia-bronchiektasis-sinusitis-syndrom (German).
泌尿 膀胱破裂分型及表现

位多见于膀胱之前壁。腹膜外型膀胱破裂多数伴有骨盆骨折。有一组1798例骨盆骨折,其中181例(10%)发生膀胱破裂。而另一组由骨盆骨折引起膀胱破裂的259例中,212例(82%)为腹膜外型破裂。47例(12%)为腹膜内型。
2.腹膜内型膀胱破裂 膀胱壁破裂伴腹膜破裂,膀胱壁裂口与腹腔相通,尿液流入腹腔,引起腹膜炎。其损伤部位多见于膀胱的后壁和顶部。
在一组100例膀胱破裂病例中,50%为腹膜外型,30%为腹膜内型,20%两型兼有。
腹部 腹膜后积气DD
(1) Traumatic rupture (usually duodenum)
(2) Perforation of duodenal ulcer
(3) Gas abscess of pancreas (usually extends into lesser sac)
(4) Urinary tract gas (trauma, infection)
(5) Dissected mediastinal air
(6) Iatrogenic
介入 腔内成形术后 内漏分类
Type 1: at the end of the graft at its attachment site with the aortic wall
Type 2: From retrograde collateral flow into the aneurysm sac by aortic branch vessels
Type 3: Through a graft defect or disconnection
Type 4: Through the graft material by increased porosity
Type 5: Endoleaks whose source is indeterminate
Types 1, 3, and 4 usually require intervention, type 2 can usually be watched, sometimes with eventual vessel embolization if the aneurysm sac is enlarging.
内漏的分型有多种,其中引用最多的是White提出的按血液渗漏部位区分的分型(2~3)它得到了血管外科学会和美国血管外科联合会(SVS/AAVS)的认同(4), 2002年,Veith等(1)又做出部分修改。
I型内漏为SG附着部内漏。因SG的近端或远端与瘤颈之间未能完全封闭,导致血流持续性流入动脉瘤腔内。又可分三个亚型:IA型和IB型分别指近、远端内漏,IC型指AUI支架中髂动脉封堵物(Iliac occluder)不严密引起的内漏。
II型内漏为返流性内漏,是因腰动脉、肠系膜下动脉和其他侧支动脉中的血流持续性返流造成的。Veith等(1)将II型内漏又进一步划分为:IIA型内漏,简单型,只有单一流入道而无流出道;IIB型内漏,复杂型,有多条流入道、流出道。
III型内漏是SG结构破坏引起的内漏,包括连接部漏、骨架脱节(IIIA);覆膜破裂(IIIB)。其中IIIB型又可根据裂孔大小分作大破口(≥2mm)和小破口(<2mm)。
IV型内漏指EVAR后30天以内发生的,SG结构完整但孔隙过大造成的内漏,30天后发生的则不包括在内。
狭义的内张力(Endotension)是指EVAR后延迟性增强CT扫描没有检出内漏,但瘤腔内张力增大的情况。广义则涵指所有瘤腔内张力增大的情形,包括各类内漏和狭义的内张力。Veith (1)等建议将其分为:A型,指即使手术也没有发现内漏;B型,指内漏已封闭或栓塞后的内张力;C型,指CT未检出的I、 III型内漏; D型,指CT未检出的II型内漏;后两种内张力只有在手术中才能证实,并主张将内张力视作V 型内漏。
内漏根据时相可划分为:术后30天以内发生的内漏称为急性内漏,30天后发生的称为迟发性内漏,在内漏自行封闭或经处理封闭后再次出现的内漏称为复发性内漏(2、3)。
2008年7月18日星期五
腹部 门脉积气 原因与简单鉴别
Recent reports have shown that portomesenteric vein gas is associated with several causes besides mesenteric ischemia. Portomesenteric vein gas is idiopathic in approximately 15% of cases. In some cases, such as those involving portomesenteric vein gas due to infectious and inflammatory abdominal diseases, interventional procedures, trauma (as in our case), and transplantation, the prognosis is favorable and surgery is not required.
Intravascular gas occurs in less than 1% of patients who sustain blunt abdominal trauma. In these patients, portomesenteric vein gas is thought to result from acute pressure changes that occur at the time of injury and force intraluminal gas into the bowel wall, where it is absorbed into the portal circulation. Portomesenteric vein gas in the setting of blunt trauma does not necessarily imply bowel necrosis or perforation, and the absence of peritonitis may allow observation of this finding.
On CT scans, air in the portal vein manifests as ramifying streaks with air attenuation that can reach the capsule at the periphery of the liver. Air has a propensity to accumulate in the intrahepatic radicals of the left portal vein due to its more ventral location. Intrahepatic portal vein gas should be differentiated from aerobilia. The distribution of hepatic gas in patients with aerobilia is central, around the portal hilum, and does not extend to within 2 cm of the liver capsule. Gas in mesenteric vein branches should be differentiated from pneumoperitoneum. Pneumoperitoneum does not have a linear, ramifying configuration and can be present in the antimesenteric border of the intestine. Findings of portomesenteric vein gas at CT should be carefully evaluated in the context of clinical findings before making decisions regarding diagnosis and therapy.
http://www.mypacs.net/cgi-bin/repos/mpv3_repo/wrm/repo-view.pl?cx_subject=6604325&cx_image_only_mode=off&cx_from_folder=92585&cx_repo=mpv4_repo
Sebastià C et al. Portomesenteric vein gas: pathologic mechanisms, CT findings, and prognosis. RadioGraphics 2000;20:1213-1224; discussion 1224-1226.
Carmen Gallego et al. Congenital and Acquired Anomalies of the Portal Venous System. RadioGraphics 2002; 22:141–159
腹部 中肠扭转 "apple-peel / twisted ribbon / corkscrew" appearance

o Usually neonate or young infant
o Occasionally older child and adult
o Duodenal atresia
o Duodenal diaphragm
o Duodenal stenosis
o Annular pancreas
o Degree of twisting is variable and determines symptomatology
o Severe volvulus (= twist of 3 1/2 turns)
§ Can result in bowel necrosis
o Bile-stained vomiting
§ Intermittent
§ Postprandial
§ Projectile
o Abdominal distension
o Shock
o Recurring attacks of nausea
o Vomiting
o Abdominal pain
o Failure to thrive (hypoproteinemic gastroenteropathy as a result of lymphatic and venous obstruction)
o Dilated, air-filled duodenal bulb and paucity of gas distally
§ "Double bubble sign" = air-fluid levels in stomach and duodenum
o Isolated collection of gas-containing bowel loops distal to obstructed duodenum = gas-filled volvulus = closed-loop obstruction
§ From nonresorption of intestinal gas secondary to obstruction of mesenteric veins
o Duodenojejunal junction (ligament of Treitz) located lower than duodenal bulb and to the right of expected position
o Spiral course of midgut loops = "apple-peel / twisted ribbon / corkscrew" appearance (in 81%)
http://radiology.rsnajnls.org/cgi/reprint/242/1/315
腹部 中肠扭转 Ladd's bands
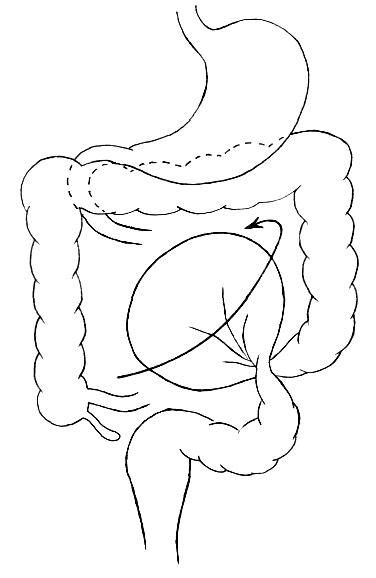
 View normal meseteric fixation.
View normal meseteric fixation.Note the broad fan of meseteric attachment of the small bowel making it difficult for a volvulus of the small bowel to occur.
If the correct rotation does not occur, it is termed "malrotation". This results in the failure of proper mesenteric development so that instead of a broad fan of mesenteric attachment, the entire midgut is attached to the posterior abdominal wall by a short, narrow stalk in the region of the duodenum. There may also be bands crossing the duodenum (Ladd's Bands) which can cause duodenal obstruction.
 View malrotation and Ladd's bands.
View malrotation and Ladd's bands.
Note the mesenteric attachment of the cecum. This narrow stalk is more prone to volvulus. Additionally, this stalk (Ladd's bands) is capable of compressing the duodenum and obstructing it.
In a malrotation, many meters of intestine are free to twist around this stalk, which, since it contains the superior mesenteric artery, is vulnerable to strangulation and ischemic necrosis. The occurrence of this twisting and strangulation results in the surgical emergency called midgut volvulus. Midgut volvulus should not be confused with cecal or sigmoid volvulus. Cecal and sigmoid volvulus generally occur in adults. Sigmoid volvulus involves the large bowel and can often be decompressed by barium enema or other non-surgical procedures.
 VIew midgut volvulus.
VIew midgut volvulus.In midgut volvulus, the majority of the small bowel is involved in the stragulation. Substantial small bowel necrosis occurs without prompt surgical intervention.
In malrotation, the cecum may be prone to twisting or kinking if it is excessively mobile. Cecal volvulus can occur in the absence of malrotation. This most often presents in adults rather than children.
 View sigmoid volvulus.
View sigmoid volvulus.Sigmoid volvulus is the most common site of colonic volvulus. It occurs most often in the elderly. It is associated with elongation of the descending colon making the sigmoid region hypermobile and prone to twisting.

